Saturday, October 5, 2013
Wednesday, July 13, 2011
Who What Where When and How-I hope someday that Advocate Health Care will be forced to answer Why
Advocate CEO, James Skogsbergh, rewarded by Mayor Rahm Emanuel
Tuesday, June 28, 2011
Jim Duffett's still taking blood money from Advocate Health Care, via his Campaign for Better Health Care
Several times I had asked to speak with Duffett, but he was always unavailable.
Now, I know why.
Tuesday, October 19, 2010
Wednesday, October 8, 2008
Like Hogan's Sgt. Schultz, Senator Dick Durbin's Policy Director, Tom Falleti, wants to know nothing.
At one point, even though he acknowledges that I was not asking Durbin's office to make a judgment about a health care quality issue, Faletti still suggests that I should solicit the opinion of doctors. I advised Faletti in my response, that a doctor's opinion is not necessary in determining if any Centers for Medicare and Medicare Services regulations have been violated.
I spoke with Faletti before faxing him my rebuttal letter. Faletti was very adversarial. Until a new president is sworn in, CMS is George Bush's agency. I cannot understand why the Policy Director of the (Democratic) Majority Whip of the US Senate, would not want to know about Bush's CMS' wrongdoing. However, Faletti defended CMS. When I offered him the documents that proved the wrongdoing, he wanted nothing to do with them. (I faxed some to him anyway.) He was adamant about not wanting to make a judgement about if there had been wrongdoing. If ignorance is bliss, then I wonder why Faletti was so cranky.
---
letter from Faletti (page one)
letter from Faletti (page two)
rebuttal to Faletti (page one)
rebuttal to Faletti (page two)
rebuttal to Faletti (page three)
Monday, September 22, 2008
Advocate executives donate to American Hospital Association PAC which in turn donates to almost everybody in Washington, DC.
George Burkstrom, of the AHA Membership Department, stated that he was not inclined to learn about wrongdoing committed by AHA members. Even though I never stated to him otherwise, he repeatedly told me that AHA would not intercede in such matters. This is one of the ways people at these institutions attempt to derail conversations. It is obvious that they do not have judicial jurisdiction over their members, but they make that an issue in order to justify their overlooking any wrongdoing committed by its members.
I reminded Burkstrom that our conversation was on the record, and then I asked him if AHA's only concern is that the members pay their dues and donate to its PAC, but he refused to answer and then he hung up on me. Of course, I knew before speaking with anybody at AHA, what its position is, but I had to give them an opportunity to provide it in their own words before writing about it. Before he hung up, Burkstrom told me that I should speak with somebody in AHA's media relations department. I left a message with that office, but I did not receive a callback.
The AHA PAC contributes money to hordes of Members of the US Senate and the US House, in fact they cover themselves evenly. All but one of the current members of the US Senate Finance Committee have received money from AHA PAC. The AHA has also contributed money to the campaigns of alleged health care advocates Senators Barack Obama, Richard Durbin, and Edward Kennedy.
Monday, August 25, 2008
Congressional workers need to get a clue.
I would like to be able to feed this into the collective minds of the said Congressional workers. They could use it for a role reversal excercise, but on second thought, I do not think that their arrogance and ignorance would allow them to be able to empathize.
Thursday, July 31, 2008
Health and Human Services Office of Inspector General gave Bette Weisberg and her crew a pass.
A month later, I received a letter from HHS/OIG that acknowledged my letter, but it stated that my complaint was against Advocate. I called the sender, Jaishiri Mehta, and advised her of the wrongdoing that CMS had committed. I told her that I would send her the corroborating documents, and that I wanted to discuss them with her. She agreed discussing them with me.
Mehta sent me a September 29, 2004 email message in which she acknowledged receiving the documents. In this email she states that she will contact me after she had a chance to look at them. That was the last that I heard from her until she sent me another email (both emails are available via the link) in response to my subsequent phone calls. In that email she contends that she cannot speak with me.
In December 2004, I received a letter from OIG "special investigator" Scott Vantrease in Chicago. The letter stated that their investigation had concluded, and that CMS personnel had done nothing wrong. I called Vantrease, and told him that there could not have been much of an investigation because I was never questioned, nor did I have an opportunity to discuss the documents with anybody.
Vantrease told me that he had more important things to do than deal with my complaint. However, he said that if I called him after the holiday, he might be able to put me in contact with somebody who might be able to resolve the matter.
On December 30, 2004, there was a message on my machine from a "special agent from Homeland Security, regarding a Health and Human Services complaint". The next day, nobody answered the phone at Homeland Security. I was not able to get a hold of the "special agent" until January 10, 2005. During that phone call, the "special agent" threatened me with "prosecution" if I did not "cease and desist" from communicating with HHS/CMS. I asked him what I had done to warrant such a threat, but he said that it was not his job to tell me. I asked him what I would be prosecuted for, and he said that he would "find something". Then he hung up on me.
It turned out that he was an employee of Federal Protective Services, which is under Homeland Security. After that one call, I never heard any more from him.
Somebody at HHS/CMS had used the Federal police force to try and scare me off from attempting to obtain the rights of my parents. I didn't get worried about the call until it became apparent that nobody that I told about it thought that it was a big deal. That is really scary.
Saturday, July 19, 2008
Advocate Health Care just kept on lying and lying and lying.
I spoke with Nancy Meyers, the Advocate nurse attending to my stepfather, about this. At the beginning of August 2003, she mentioned that my stepfather was not doing well in therapy, and that he would probably have his benefit suspended soon. My bypass surgery had already been postponed several times by this point, and I told Myers that it was important for me to know when my stepfather would have to leave Warren-Barr, so that I could make plans for his care while I was recuperating. If my stepfather had been able to assist himself, there would not have been a problem in having him come home. However, Myers had been saying that he may never walk again, and so he needed somebody to care for him while I recuperated. (for example, I was not supposed to lift anything heavy so my chest could heal.)
My August 20 surgery was again postponed...on August 20. Advocate had no way of knowing this. That morning, I received a call from a friend whose number I had given out for emergency purposes. Somebody from Warren-Barr had called him and had told my friend that my stepfather's PT was going to be terminated on August 22, 2003, and they wanted to know where my stepfather would be going. After hearing, this I immediately called Dr. Rajan Raj, his surgeon, and he told me that the PT that my stepfather had received had not been adequate. I asked if he would put that in a letter, and told me that he would. (However, it took about four months before he wrote one.)
The sleazy charlatans of Advocate really out did themselves this time. First, they lied to me about when my stepfather would have his PT terminated. Then they waited until the day that they thought that I would be having quadruple bypass surgery to make the announcement that two days after my planned surgery, his PT would be terminated.
Thursday, July 17, 2008
Faith based not for profit Advocate Health Care...ya wanna buy a bridge?

Wednesday, July 16, 2008
Today's vocabulary lesson features the term "blood money". It means compensation paid to the family of somebody who has been killed.
Funny, I do not see Advocate's name on the list of Health Care Justice Endorsers.
I wonder if Jim Duffet, the founder of CBHC, has installed red lights outside of his offices.
Monday, July 14, 2008
Former CMS employee Bette Weisberg allowed Advocate's involuntary disenrollment of the beneficiaries.
I called Seo's office, and spoke with one of the nurses. She told me that the decision had nothing to do with Seo, but was in response to my having filed a complaint with the Illinois Department of Professional Regulations against two Advocate doctors, David Kushner and Abkar Khan.
Kushner had been my mother's hospitalist (attending physician) at Advocate Lutheran General Hospital when she was admitted there in April 2003. He was one of the doctors who ignored her medical history, and inspite of my protests, he took her off of a medication.
My mother had not been eating because she was in a great deal of back pain. Kushner told me that he had taken her off the medication because it causes anorexia. I explained to him that it was the pain that was causing her "anorexia", but he ignored me. He also refused to consult with the specialist who had prescribed the medication.
Prior to her hospitalization for the back pain, the biggest problem that we had had with my mother was that she would try to walk around without her walker. After two days in Lutheran General, she was rendered incontinent, and was never able to walk again. She eventually had to be placed in a nursing home.
Khan was the attending physician at Governor's Park in Barrington, IL. That was the nursing home she was sent to ostensibly for sub-acute physical therapy. She had been discharged from the hospital after two days, and had been diagnosed as having a compression fracture in her back. I never was given any proof of this, and had I not been busy having a heart attack, I would have appealed her being discharged so soon.
While at Governor's Park, she was given so much pain medication, that she was somnolent. Consequently, she was not enthusiastic about doing any physical therapy. She did have a history of mild multi-infarct dementia, which was exacerbated by the drugs. I pleaded with Khan to intervene, but without any luck. There were many more problems at Governor's Park, but since I was not as famiiar at that time with the Appeals process, I made some errors in reporting the problems.
Considering that CMS did not enforce the regulations about Appeals, I do not know if I would have had any luck if I did make my complaints about Governor's Park properly.
She was first discharged from Governor's Park in May 2003, at which time she was so doped up that she could not sit up in the car. I brought her from the back of the place to the front, and requested that she be checked back in. They did so as a "favor", but only for several days, until I could find a nursing home to place her in.
It is important to mention that the staff at Governor's Park were insistent that she had Alzheimer's. They ignored me when I told them that the drugs were causing her to be so confused. On top of that, I later found out that she had had a bladder infection while at Governor's Park, and that that could have contributed to her confusion too.
I found a nursing home to place her in, because there was no way that I could have attended to her at home anymore. She survived two years there, and I will touch on that in another post. However, after about a month or so, she was finally backed off on the abundance of meds that she had been prescribed in Governor's Park, and literally within a day or so her cognitive ability bounced back. Unfortunately, she remained incontinent and unable to walk.
CMS had to approve my folks being disenrolled from Advocate, and Weisberg once again gave Advocate her blessing. Her account of why they were disenrolled was in line with Advocate's official (fact free) reason, and the language that she used to describe the reason sounds like collusion. In a August 2004 letter to me, Weisberg wrote that my "behavior" had caused my folks to be kicked out of the network. She just could not resist getting in a dig at me.
More CMS BS from Weisberg
Sunday, July 13, 2008
Former CMS staff member Bette Weisberg enabled Advocate to dodge explaining health care decisions.
The following is from Chapter 13 of the Medicare Managed Care Manual.
The manual provides an example of unacceptable language and the acceptable language that is to be used. The criteria and rationale should be restricted to the progress of the patient, not generic and rambling CMS definitions. For example, a correct written response might look like the following.
• The case file indicated that while [Stepfather] was making progress in his therapy programs, his condition had stabilized and further daily skilled services were no longer indicated. The physical therapy notes indicate that he reached his maximum potential in therapy. He had progressed to minimum assistance for bed mobility, moderate assistance with transfers, and was ambulating to 100 feet with a walker. The speech therapist noted that his speech was much improved by 6/12/2001, and that his private caregiver had been instructed on safe swallowing procedures and will continue with feeding responsibilities.
This level of information has never been provided to us by Advocate, and it had made countless decisions over the years about my stepfather and mother's health care. In fact, the only written notification we were ever given, was always done with "unacceptable" language.
I informed Lee B. Sacks and Dan Schmidt at Advocate about this. (Sacks is the Chief Medical Officer, Schmidt the President of Advocate Health Care.) In response, Schmidt had an assistant send me some generic crap about skilled nursing facilities. That shows the amount of contempt that Advocate holds toward its beneficiaries. Sacks weighed in with the same inane comments, and I think that he should lose his license to practice medicine. Finally, I was summarily dismissed by former Advocate Assistant General Counsel, Thomas Babbo.
Of course, this was all totally acceptable to Weisberg.
What this all means is that Advocate never had to explain the medical criteria and rationale, particular to my folks, that was used in making decisions about their health care. I think that that is a good thing for Advocate, since those decisions seemed to be more concerned with its bottom line than the well-being of my folks.
I liken Advocate Health Care to an organized crime organization.
------------------------------------------------------------
Note: I have edited out the name of the HMO because I have determined that Advocate deceived it, as much as Advocate deceived us.
The following are links to the first letter that I wrote to Advocate's Chief Medical Officer, Lee B. Sacks, MD, in 2004.
The following is a link to a copy of the letter that I faxed to Dan Schmidt as a follow up to my phone call with him.Letter to Schmidt
The following is a link to a copy of the letter that I faxed to Assistant General Counsel Thomas Babbo in response to his August 20, 2004 letter to me. It did not render a response.
Letter to Babbo.
Saturday, July 12, 2008
Advocate's money vs. my folks' lives...no contest.

Former CMS employee, Bette Weisberg, enabled Advocate to violate numerous CMS regulations.


I supplied Weisberg with an abundance of written and audio testimony, as well annotated documents, that clearly showed that the Advocate had repeatedly failed to abide by numerous CMS regulations. Weisberg did not dispute the testimony and documents; she refused to acknowledge their existence!
My stepfather had surgery late in June 2003 at Advocate Lutheran General. His surgeon had informed me that he wanted my stepfather to receive acute physical therapy at Lutheran General’s 6th floor rehabilitation unit after his surgery.
I was informed by the hospital staff members that my stepfather would be evaluated to determine if he fit the criteria for acute PT. (Acute PT is intensive.) I was later told that he had been evaluated and had been found not to be a candidate for acute PT. I was then advised that he would be sent to a skilled nursing facility where he would receive sub-acute PT. I did not file an Expedited (Fast) Appeal, because I had been told that acute PT would be too rigorous for him.
In March 2004, I found out that my stepfather had never been evaluated for the acute PT. Another Advocate employee advised me that he did not receive the acute PT because the HMO (insurance company) would not pay for it because the service was “out of network”. (This individual did not realize that she was blowing the whistle on Advocate, her employer.) She arranged for me to receive a copy of his evaluation form, which had not been included in his medical records that I had obtained after his surgery. Advocate had lied to me in order to prevent me from filing a Fast (Expedited) Appeal. I will never know if the insurance company had advised Advocate that the 6th floor rehab center was not a part of my stepfather’s network. (I think Advocate lied about that too.)
I brought this to the attention of former CMS Region V Medicare managed care manager, Bette Weisberg, and her crew. I provided Weisberg with a copy of the evaluation form, but she refused to acknowledge its existence. Instead, she claimed that no service had been denied. She even went so far as to claim that there was no such thing as acute PT!
The following has been on the CMS website since at least 2003.
Medicare Appeals and Grievances
Your Medicare Appeal Rights:
Unfortunately, nobody I have contacted is interested in making anybody at CMS accountable for Weisberg and her crew's illicit actions.
Thursday, June 26, 2008
I can be AARP's - Divided We Fail friend on My Space, but I am not allowed to talk to its policy makers.
Initially he kept directing me toward the Divided We Fail web site, and the “Share Your Story” feature. I advised him that that was a nice way for AARP to get people to feel involved, but that I wanted to do something more than tell anecdotes. He also mentioned that AARP – Divided We Fail has both a My Space and a Facebook account. I told him that I was not calling to find a date.
He then said that there were numerous gatherings where individuals could provide input. After repeatedly asking him to give me some examples, he finally gave me two, however, the gatherings he referred to had not had anything to do with Divided We Fail other than Divided We Fail had been “invited to attend”.
Finally, he admitted that there is no way that an AARP - Divided We Fail member can meet “one on one” with an AARP - Divided We Fail employee (policy maker). I told him that a literal “one on one” meeting would be nice, but that I would also be interested in being able to speak with the policy makers via a group of other people, as long as the meeting was limited to AARP - Divided We Fail business. He told me that that was not possible, but refused to tell me why. Then he referred me back to the Divided We Fail web site and the “Share Your Story” feature, after which he then hung up on me.
Note-
I told Mr. Cardenas that I initially had been referred to Ms. Terri Worman, Associate Director, AARP Illinois, but that she had not responded to my voice mail messages or my email. I mentioned that I had searched her name via Google, and learned that her expertise is that of a community organizer for the GLBT community, especially for the senior citizens who are a part of that demographic. Cardenas interpreted my comment as being a personal attack on Worman. I explained to him that I was just repeating the information that praised Worman and that I had read on the Internet, but Cardenas insisted that it was a personal attack.
Next I called AARP's main number again and asked a very nice operator if there were any other offices that I could call to get my questions answered, since I was not having any luck with the Illinois office. She told me that she has been told to direct people only to their state offices, and that she did not have a number for a national office.
That means there are fifty state offices divided up amongst the US. I guess that "Divided We Fail" is an appropriate name for this organization.
According to AARP, "Divided We Fail (www.dividedwefail.org) is a national initiative led by AARP, Business Roundtable, Service Employees International Union and the National Federation of Independent Business, to give a voice to millions of Americans who are tired of letting Washington gridlock stand in the way of affordable, quality health care and long-term financial security. Common sense solutions are needed, and everyone – individuals, businesses and government – has a role and a responsibility in ensuring health and financial security for all."
AARP is the only organization that I am entitled to join.
Wednesday, June 25, 2008
Another reelection campaign and another letter requesting Melissa Bean to be accountable for her House staff.

 This letter was faxed to Melissa Beans House office in Washington DC on June 25, 2008. I will note here whether or not it renders a response.
This letter was faxed to Melissa Beans House office in Washington DC on June 25, 2008. I will note here whether or not it renders a response.Email to Terri Worman, AARP Illinois Executive, regarding Divided We Fail
.JPG)

On June 20, 2008, I was informed by numerous AARP employees via my phone inquiries, that Ms. Terri Worman is the AARP employee who will answer any questions that I have about the AARP program, Divided We Fail.
I left a voice mail message for Ms. Worman last Friday, June 20. Her outgoing message stated that she was out of her office, but that she would be returning to her office and returning calls on Monday, June 23.
I mailed her the email posted above on Tuesday, June 24.
I have not heard from her yet.
Health care advocate/mercenaries get press in the Chicago Tribune
I once spoke by phone with Ms. Graham, in an attempt to tell her about my experience serving as a health care advocate on behalf of my folks.
However, Graham was not interested. I had explained to Graham that I was not seeking publicity, but that I wanted simply to convey my experience. The aforementioned article is a good example of why I thought that a reporter would be interested in learning about the wrongdoing that I have encountered.
There is not really a “health-care maze”. If I was able to figure it out, then any reasonably intelligent person should be able to figure out how to handle any health care issue. Doing so is time consuming, but not that complicated.
The problems that I ran into were not due to a “maze”, but rather because my folks' Medicare managed care provider used deceit to dodge the Medicare managed care regulations. The regulations are supposed to be enforced by the Centers for Medicare and Medicaid Services; they have been established to prevent the Medicare managed care policyholders and providers from placing their bottom lines above the well-being of the beneficiaries. In our case, CMS has given the provider its approval for dodging the regulations.
According to Graham, “The field is known as "health-care advocacy”, and services typically assist with everything from resolving insurance disputes to researching treatment options to connecting people with medical resources.” This is all done for a fee, ranging anywhere from “$395 a year” at one company, to “$200 an hour” at another.
One of the companies mentioned is “an upscale solution, serving as the health-care equivalent of an exclusive, high-end private banker for more than 3,600 clients.” Graham writes that, “Today, at least 20 families on Forbes' list of the richest Americans are clients, paying from $10,000 to upward of $50,000 a year for a PinnacleCare membership.”
Graham provides an example of a man who purchased the services of PinnacleCare for his wife and three adult children. She writes, "Late last year it cost $41,000 a year for a VIP package for himself and his wife, ensuring that a top-notch physician would oversee all their medical needs; $30,000 a year for a package focused on healthy living for his three adult children and their families; and $21,000 for a one-time fee to compile comprehensive electronic medical records for everyone.
In all, that's $92,000 paid on health-care advice by this 66-year-old entrepreneur before a dollar was spent on medical services actually delivered."
These companies advocate because they make money doing it. I advocate because it is my folks that need the help. I do not know what PinnacleCare does that I have not done, but I sure would like to find out what they do for $50,000 a year.
I wonder if my folks had been wealthy, if that would have made a difference in how the provider chose to abide by, and how CMS chose to enforce, the CMS regulations.
If Graham had bothered to take a little bit of time to learn about my experience as a health care advocate, she might have wondered the same thing.
-----
Note:On June 22, I sent an email to Ms. Graham, in which I reminded her that I had tried to tell her about some of my experiences, but that she had not been interested. She wrote me back almost immediately, and stated that she has talked with a lot of people, and that she was sorry if she had offended me.
Monday, June 23, 2008
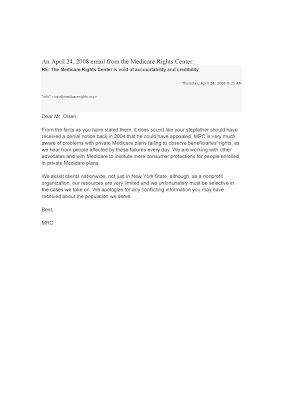
Medicare Rights Center anything but


“History
The Medicare Rights Center National HMO Appeals Hotline, in operation since September 1997, provides direct assistance to older and disabled people who have had necessary care denied, reduced or terminated by their Medicare HMO. From September 1999 through August 2000, MRC's HMO Appeals Hotline handled 709 cases, secured much needed care for our clients, and saved them over $360,930 in out-of-pocket costs.
The Appeals Process
Our counselors guide callers through the HMO appeals process and, when necessary, intervene on their behalf with Medicare HMOs. After getting basic information about the problem, MRC staff either provide clients with information about how they can handle their own appeal or intervene directly on behalf of clients with their HMOs. In the typical case in which MRC intervenes on the client's behalf, hotline staff telephone the HMO to gather information and to advocate informally for our client.
When informal advocacy fails, MRC may write a letter to the HMO asking it to reconsider its denial. These letters contain facts, regulations and supporting documents pertaining to the case. MRC routinely sends a copy of this letter to the appropriate Health Care Financing Administration regional office, since we believe it is important to keep HCFA apprised of individual problems in a particular HMO as well as systemic problems that we observe when a large number of our callers run into the same difficulty.”
(The Health Care Financing Administration, or HCFA, became the Centers for Medicare and Medicaid Services in 2001)
One would think that an organization claiming to “institute more consumer protections for people enrolled in private Medicare plans”, would welcome well documented testimony about the wrongdoing perpetrated by a major private Medicare plan, with the blessing of the Centers for Medicare and Medicaid Services.
Furthermore, one would think that such an organization would post on its website, the criteria required in order to receive its assistance.
Neither is the case.
For at least a decade, my folks’ Medicare managed care HMO has referred its beneficiaries to the Medicare Rights Center for assistance in filing appeals. (This is true as of June 18, 2008.)
However, we have been repeatedly refused such assistance by MRC. The reasons have varied.
In 2003, the first time that I called MRC’s hotline on my folks’ behalf, a recording advised me to leave my name and number, and I received a phone call shortly after, but I was told by that individual that she did not know how MRC could help us. I had called MRC because my (late) mother’s Medicare provider had failed to provide her with medical services that her medical history, including the opinions of the specialists who had seen her, deemed necessary.
I called MRC again in mid 2004, on behalf of both my stepfather and mother for the same reason, and according to the Centers for Medicare and Medicaid Services website:
“Your Medicare Appeal Rights:
You have the right to appeal any decision about your Medicare services. This is true whether you are in the Original Medicare Plan, a Medicare managed care plan, or a Medicare prescription drug plan. If Medicare does not pay for an item or service you have been given, or if you are not given an item or service you think you should get, you can appeal.”
This time I was told via a phone call with MRC’s former Director of Client Services, Rina Kitazawa, that MRC only assists residents of New York State. I informed Kitazawa that in my stepfather’s case, I had found out that the Medicare provider had lied to us about the reason he had been denied a service, but she told me that there was nothing that she could to assist us.
Inexplicably, on or about the fall of 2004, I received a phone call from somebody at MRC saying that somebody was going to be getting in contact with me regarding my stepfather’s case. As it turned out, nobody contacted me.
I wrote a December 12, 2004, letter to Kitazawa asking her to clarify the requirements needed to receive assistance from MRC. I received a letter dated January 14, 2005 that was completely void of fact. Instead of answering my question, for some reason Kitazawa had decided to claim that MRC had carefully examined our case and had determined that we had nothing to appeal!
Earlier, I had provided Kitazawa with documents and testimony that showed that my stepfather’s surgeon (who was employed by the Medicare managed care provider) had requested that my stepfather be given acute physical therapy in my stepfather’s HMO network hospital (which was owned by the Medicare managed care provider) after my stepfather had neck surgery.
I had been told at that time that my stepfather had been evaluated to determine whether he was a candidate for acute physical therapy, and that it had been determined that he was not a candidate.
However, later I found out that he had never been evaluated because according to the Medicare managed care provider, the Medicare managed care HMO would not approve the service because it was “out of network”. (This was a service denial, and thus subject to appeal.) This information had been withheld from his medical records.In her letter to me, Kitazawa knowingly took a position based on the Medicare managed care provider’s deception. Kitazawa refused to acknowledge the documents that showed that a service had been denied.
I have had no further correspondence with Kitazawa. She is no longer at MRC.
The Medicare managed care HMO continued to list MRC as a resource for beneficiaries to use for assistance in filing appeals, and in late 2006, I spoke via a phone call with Paul Precht, MRC’s Director for Policy and Communications in Washington D.C.
Precht informed me that the Medicare managed care HMO was in error for referring its beneficiaries to MRC, but he refused to put that in writing, nor would he allow me to record our conversation.
There are many people, especially those affiliated with MRC, who believe that there is a statute of limitations regarding accountability. I have written to Robert Hayes, President and General Counsel MRC, requesting an explanation, and I have never received a response.
In June 2008, I phoned one of the foundations that grants funds to MRC. I spoke with Barbara Geenburg, President of The Philanthropic Group in New York. According to its website she “designed the grantmaking strategy for the Helen Andrus Benedict Foundation, and directs its grantmaking program.”
I started our conversation by telling her that I was concerned about the manner in which MRC advertised itself. Instead of responding to my concern directly, she asked me why I was talking about something that happened some years ago. I told her that it was because MRC was still allowing the HMO to use its name as a source for assistance. She then told me that she did not think that MRC could get the HMO to stop. I told her that that was ridiculous. She then asked me, as if she were his assistant, if I wanted Hayes to call me. I gave her my phone number, however, I still have not heard from him.
MRC’s promotion of itself has been very successful. Scores of other organizations have also referred me to MRC for assistance with appeals. Some individuals have insisted that I must be mistaken about MRC’s refusal to assist us. One of the reasons MRC’s lack of integrity is harmful is because there are so many people who believe its hype!
In our case, I wasted valuable time contacting and waiting for responses from MRC, because I believed their hype too. There is a need for legitimate resources to be made available to people like us.
The information that MRC offers via its website is available elsewhere on the Internet on sites such as those belonging to WebMD and CMS.
I believe that MRC’s principals hope to keep the donations and grant money coming in by continuing to make false claims about the scope of their assistance to Medicare and Medicare managed care HMO beneficiaries. There is no other reason for them not disclosing the limitations that they have personally disclosed to me.
(MRC’s most recent IRS 990 forms are available for free at GuideStar . Registration is required, but there is no cost to examine the forms.)
Sunday, June 22, 2008
Congresswoman Melissa Bean (D-IL, Eighth District) needs to be accountable for herself as well as her congressional staff.
In February 2005, on behalf of my stepfather and now deceased mother, I provided Jordan with scores of written testimony and annotated documents, which showed how a Medicare managed care organization had circumvented numerous Medicare regulations with the blessings of Health and Human Services and the Centers for Medicare and Medicaid Services. The fact intensive information that I gave to him was not complicated, but there was a lot of it, and I offered to meet with him if he needed assistance in understanding its significance. Jordan was not enthusiastic about meeting with me, and he did not have an understanding of what a Congressional caseworker may do on behalf of a constituent.
My knowledge of the guidelines for Congressional caseworkers comes from the US House Ethics Committee, as well as other US government publications. This information is readily available via the Internet.
The following statements are from the US House Ethics Committee (Committee on Standards of Official Conduct).
Members and staff of the House often assist constituents in their dealings with administrative agencies by acting as facilitators or "ombudsmen". Members may properly communicate with agencies on behalf of constituents:
* to request information or status reports;
* to urge prompt consideration of a matter based on the merits of the case;
* to arrange for appointments;
The failure of a regulatory agency to enforce its regulations obviously fits into the category of what issues “Members” may inquire about. However, Jordan inexplicably told me that he could not even express judgment about the matter to me, let alone HHS/CMS.
One of the specific violations that I reported to Jordan was that CMS and the Medicare managed care provider had repeatedly denied my stepfather and mother, in a variety of ways, their right to make Appeals, expedited (fast) and otherwise (i.e. due process).
Initially, Jordan was unable to grasp that the issue was not about a judicial matter that I wanted Bean to intervene in. He had trouble understanding that there was no judicial matter because we had been denied access to the regulatory judicial process!
I had told Jordan that I would not turn down any offer of assistance in resolving the matter. However, I also told him that my goal was to convey the wrongdoing that I had encountered to Bean via her staff. I had hoped that somebody in her office would have taken the time to look at the material that I provided to them, and understood what the HMO and CMS had done that was wrong. I thought that this was important, because Bean was going to be voting on Medicare related bills. The Appeals process is the most important safeguard that has been established to protect beneficiaries from having their healthcare compromised by the bottom line of the Medicare managed care insurer and its provider. I had hoped that Bean and her staff would be interested in learning about how CMS was allowing the regulations regarding the Appeals process to be violated. That hope turned out to be wishful thinking.
Jordan eventually mailed a "letter of inquiry” regarding the issue, but:
• He mailed it to the wrong place,
AdminiStar Federal, a company that has a contract with the Federal government to oversee the policies of beneficiaries enrolled directly in MedicareJordan had told me that he was going to send a letter to AdminiStar Federal. I then had advised Jordan that instead he should direct any correspondence to Matthew Brown, who at that time was the CMS Congressional Liaison in Washington. I explained to him that my stepfather and my mother were Medicare + Choice (now Medicare Advantage) beneficiaries, and CMS itself oversees those policies. Jordan chose to ignore me.
(By definition, any issues involving the CMS Appeals process will have origins in medical procedures, but I stated in writing to Jordan that I was not asking him to address that issue.)
Because Jordan misidentified the issue as being about the quality of healthcare, AdminStar Federal forwarded the letter from Bean/Jordan to my parents’ Medicare + Choice HMO (the insurer) that had a contract with the Medicare managed care provider). Quality of care issues are formally called Grievances, and at that time were handled internally by the HMO.
Everything that took place next is based on hearsay, as written by Jordan, and his story is absurd. (That is what happens when people do not tell the truth.) He claims that an (as yet) unidentified person or persons at the HMO then voluntarily forwarded the letter to an (as yet) unidentified person or persons at an (as yet) unidentified location at “CMS”. According to Jordan, he then received a phone call from an (as yet) unidentified person or persons from CMS, advising him that the “answers” were the same. Jordon refused to specify what the answers were, or what questions these “answers” were in response to. He won't identify the concerned parties either.
I voiced my concern about this via a phone call with John Gonzalez, Bean’s Chief of Staff, on June 30, 2005. Gonzalez told me that he would look into the matter and get back to me after the Fourth of July holiday, but I did not hear from him again.
It might be unreasonable for Bean to be held accountable for the actions of her caseworker, but she has to be accountable for her chief of staff. Unfortunately, Bean has not been made accountable for much of anything. If Congresswoman Bean is concerned about congressional accountability, she should start by being accountable for herself and her congressional staff.
If our votes count, then Bean should be concerned about losing ours.
Illustrations
1. I dropped off the testimony and documents at Bean's office in February 2005, and I faxed this follow up letter to Bean's district office manager in March 2005.
2. The June 16, 2005 letter from Bean with the result of the "letter of inquiry".
3. Nicholas Jordan mailed the "letter of inquiry" to the wrong place (Administar Federal) and misidentified the issue as being about "[health] care".
4. The response letter from Administar Federal to Bean. Because Jordan misidentified the issue as being about the quality of care received by my folks, Administar Federal correctly forwarded it to the insurer. A complaint about the quality of care is a Grievance, and at the time was handled internally by the insurer. Yet, the letter refers to "services" not delivered which is an Appeals issue. If anything, the letter shows that thanks to the people involved, the system consists of nothing but weak links.
If Jordan had correctly identified the issue as being about CMS' failure to enforce its regulations, Administar Federal might have forwarded the letter to the correct location, the office of the Congressional Liaison, in Washington DC.
5. In October 2005, I requested copies of all of the correspondence that had been generated by Jordan's letter of inquiry. I received this letter along with the two previous ones linked to in items 3 and 4. Jordan still would not specify the "answers" that he claimed to have received ex parte from the unnamed person or persons at CMS.
Tuesday, April 22, 2008
Waiting for a response from the office of Senator Dick Durbin (D-IL) for almost four years


Update September 22, 2008: Several weeks ago I received a letter from Durbin's policy director, Tom Faletti. As has been the case with most of the employees of the politicians and government agencies that I have corresponded with, Faletti's letter was void of fact. (There must be an epidemic of lower gastrointestinal issues in Washington DC, because most of the information that those people come up with is that which they pull out of their butts.)
I then spoke with Faletti , but he was adament about not wanting to take the time to learn the facts. On top of that, he repeatedly asked me what I wanted him to do, even though I repeatedly told him that the only thing that I wanted him to do was to take the time to learn the facts.
I followed up our conversation with a letter that rebutted his written comments. I will wait a few more weeks to see if he responds, before I post his and my letter.
Tuesday, March 25, 2008
Letter to Chicago Tribune Editorial Board
March 25, 2008
The Chicago Tribune
attn: Tim McNulty
435 N. Michigan Av.
Chicago, IL. 60611-4041
Dear Mr. McNulty:
For the past four years, I have been trying to share my experience in dealing with my stepfather’s and late mother’s Medicare Advantage HMO and Advocate Health Care (including Lutheran General Hospital), as well as Health and Human Services/Centers for Medicare and Medicaid Services. I have also written numerous letters to “Voice of the People”, none of which were published online or in the paper.
I started overseeing my folks’ health care needs about a decade ago, and became their live-in full-time caregiver in 2000.
Medicare Advantage HMOs have the right to deny specific medical procedures; however, the beneficiaries have the right to make appeals, expedited and otherwise, in response to any denials. Furthermore, according to CMS, a beneficiary can make an appeal simply because they think that they did not receive “an item or service” that they think that they should have received.
Medicare Appeals and Grievances
Your Medicare Appeal Rights:
You have the right to appeal any decision about your Medicare services. This is true whether you are in the Original Medicare Plan, a Medicare managed care plan, or a Medicare prescription drug plan. If Medicare does not pay for an item or service you have been given, or if you are not given an item or service you think you should get, you can appeal. (emphasis mine)
Appeal Rights Under the Original Medicare Plan:
If you are enrolled in the Original Medicare Plan, you can file an appeal if you think Medicare should have paid for, or did not pay enough for, an item or service you received. If you file an appeal, ask your doctor or provider for any information related to the bill that might help your case. Your appeal rights are on the back of the Explanation of Medicare Benefits or Medicare Summary Notice that is mailed to you from a company that handles bills for Medicare. The notice will also tell you why your bill was not paid and what appeal steps you can take.
Appeal Rights Under Medicare Managed Care Plans:
If you are in a Medicare managed care plan, you can file an appeal if your plan will not pay for, does not allow, or stops a service that you think should be covered or provided. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision. The plan must answer you within 72 hours.
The Medicare managed care plan must tell you in writing how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan does not decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan. See your plan's membership materials or contact your plan for details about your Medicare appeal rights.
For more information about the grievance, organization determination, and appeals processes under Medicare Managed Care, see the Medicare Managed Care Appeals & Grievances webpage on the cms.gov website: http://www.cms.hhs.gov/MMCAG
In our case the HMO had subcontracted with Advocate Health Care to deliver the health care, and to also act as an HMO. Advocate circumvented the appeals process numerous times, in a variety of ways, and they did so with the blessing of HHS/CMS.
I have spoken and written about this matter to a slew of politicians, employees of numerous self-described advocacy groups, lawyers, law students, and members of the media. The apathy and ignorance I have encountered has been both troubling and surreal.
The Tribune has endorsed mandatory health insurance. I think that that is one very good reason why somebody at the Tribune should make note of what I have to say. I have a very well documented case to make.
A Tribune editor once commented to me, “Everybody thinks that they have these great stories!”, prior to her blowing me off. One Tribune reporter has always been too busy writing about health care to provide me with an audience, while another reporter simply has not appeared to understand what I was talking about.
A reporter for WBEZ once told me that they would not be interested in one family’s experiences, and thus they would need examples of wrongdoing experienced by others. I told him that he was the reporter, and that since my claims were well documented, he might consider using them as a stepping-stone to look into the matter. I guess that he considered that idea as being too much work.
A reporter for the Sun-Times did not bother to look at the documents that I had sent to her, but she did bother to advise me, “This sounds like an arcane dispute with an insurance company.” That was the dumbest thing that anybody had said to me about the matter, and I told her so. I do not know why any media outlet would want to employ people who are so arrogant. They are merely reporters, and as such one would think that they would not want to cut themselves off from information from “the street”.
There was only one media employee whom I had spoken with that I think had any integrity. He was a Sun-Times editor who quit several weeks ago in response to the layoffs. He had told me that he did not have the financial support to assign such a story. I do not think that he would have needed all of the people that he claimed that he would need, but what he said sounded sincere and thus much different than the [stuff] that I had heard from so many others.
I am not seeking publicity for my folks, but I think that it is important for you to understand that the safeguards that have been established to protect the beneficiaries are not working, thanks mostly to CMS.
Having health insurance is no guarantee that the beneficiary will receive the appropriate health care, and you need to report that…somehow…especially since you are in favor of mandatory health insurance.
Sincerely,
John H. Olsen
cc: all members of the Tribune editorial board.
Update:
No response as of June 23, 2008
